It’s time for clarity on this misunderstood eating disorder.
A condition first identified in the 1990s, orthorexia nervosa profoundly disrupts the lives of men and women of all ages, and most don’t even know they have it. Often, their doctors don’t either. On the contrary, healthcare professionals often praise their patients with orthorexia for their “healthy” diets.
Orthorexia is derived from the Greek orthos meaning “right” and orexia meaning “appetite,” and translates as “righteous eating.” People with orthorexia are obsessed with pure, proper, healthful eating—paradoxically to the detriment of their health and well-being.
They become so fixated on their healthy diets that they severely restrict the types of foods they eat, the people they eat with, and the places where they buy or consume their food. The obsession with food quality may lead to people casting aside entire food or nutrient groups because they’re believed to be “impure” or “unclean.” This restricts a person’s overall food intake, which may lead to undernourishment, fear of weight gain, body image obsession, and restrictive eating disorders.
Eating disorder expert Steven Bratman, MD, coined the term “orthorexia” in the late 90s. He famously called the condition “a disease disguised as a virtue,” which captures well the psychology that underpins orthorexia.
The condition is similar in some ways to anorexia and obsessive-compulsive disorder (OCD), and in fact, people can have these conditions simultaneously. When that happens, each of the co-occurring illnesses becomes exponentially harder to treat.
The particular challenge of orthorexia
Again, what makes orthorexia so hard to treat is that people often don’t know they have it. They believe they are role models of physical health and don’t need help. Everyone tells them “you’re so good!” because of their clean eating. They feel validated.
Therefore, very few people go to the doctor and say, “Doc, I think I may have orthorexia.” Rather, their healthy-eating obsession makes them feel self-righteous and superior to “average” American eaters.
Unfortunately, many doctors end up agreeing with them. That’s because eating disorder training is still not a high priority in most medical schools despite increasing rates of eating disorders over the last two decades—and more acutely since the COVID pandemic. Too few healthcare providers are able to identify eating disorders in their patients, and even if they do identify them, providers struggle to successfully intervene.
Most doctors are far more comfortable fighting the “war on obesity.” This often causes them to focus too narrowly on weight and BMI at the expense of more reliable indicators of health such as blood pressure, cholesterol levels, blood glucose, quality of life, level of engagement with exercise and movement, and overall mental health.
A damaging side effect of that focus is that it perpetuates weight stigma. This causes people with larger bodies to avoid healthcare altogether and to seek unsustainable diets as a solution to their problems. This leads to worsened physical and mental health in the long run, and a greater risk of developing an eating disorder.
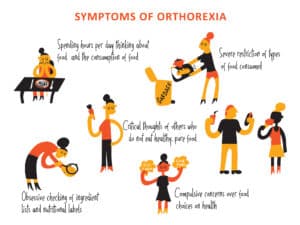
Warning signs and symptoms of orthorexia
Here’s how orthorexia often presents itself:
- Compulsive checking of ingredient lists and nutritional labels.
- An increase in concern about the health of ingredients.
- Cutting out an increasing number of food groups (for example all sugar, all dairy, all animal products).
- An inability to eat anything but a narrow group of foods that are deemed “healthy” or “pure.”
- Going to four different grocery stores to find “clean” ingredients for the food you want to prepare.
- Spending hours a day thinking about what food might be served at upcoming events.
- Showing high levels of distress when “safe” or “healthy” foods aren’t available.
- Obsessive following of food and healthy-lifestyle blogs on Twitter, TikTok, or Instagram.
Video: An Individualized Approach to Treating Eating Disorders
Dr. Sita shares her expertise in treating eating disorders.
Risk factors for orthorexia
Risk factors vary, but generally fall into three main groups:
- Biological: Having a close relative with an eating disorder, or a history of dieting or type I diabetes.
- Psychological: Perfectionism, obsessionality, dissatisfaction with your body, or a history of anxiety.
- Social/cultural: Being teased or bullied about your weight, fixating on the idea of an “ideal” body, or experiencing family trauma that spans generations (as with Holocaust survivors, alcoholism in the family, intergenerational cycles of abuse, systemic oppression).
What orthorexia looks like: a hypothetical case
In a recent article published by the National Institutes of Health, study author Jonathan R. Scarff, MD, created a helpful composite of an orthorexia patient. Meet Mr. P, who has orthorexia:
Mr. P is a 30-year-old male who has wanted to “be healthy” since childhood and who focuses on exercise and proper diet. Unfortunately, his anxiety about his diet and food intake has steadily increased. Two years ago, he adopted a vegetarian diet by progressively eliminating several foods and food groups from his diet. He now feels “proud” to eat organically grown fruits, vegetables, nuts, and beans, and drink only fruit or vegetable juice.
He spends three to five hours a day preparing food or talking to friends and family about the “correct foods to eat.” He feels significant guilt and shame whenever he “slips up” on his dietary regimen by eating seafood, beef, or pork products. He makes up for these slips with a full day of fasting.
He refuses to go to restaurants and has started declining offers from friends to eat dinner at their homes unless he can bring his prepared food. He describes feeling “annoyed” when he sees other people eating fast food or meat.
A self-test to help you diagnose orthorexia
If you suspect that you or a loved one may be heading toward orthorexia, this brief quiz can help clarify the next steps:
- Do you ever wish you could stop thinking so much about food and spend more time thinking about your loved ones?
- Are you constantly questioning food and considering how foods are unhealthy for you?
- Do you feel guilt or shame when you stray from your perfect diet?
- Does it seem physically impossible to eat a meal prepared by someone else?
- Do you feel in control when you stick to your planned, healthy diet?
- Do you look down on others who eat less healthfully than you?
If you answered yes to some or all of these questions, contact a provider with expertise in orthorexia or eating disorders in general. SunCloud Health offers treatment for orthorexia and other eating disorders.
Treatments for orthorexia
At this point, there are no clinical treatments that were specifically developed for orthorexia. However, many experts treat orthorexia with therapies that are helpful for treating anorexia or OCD.
A key goal of therapy is to help you realize that even though eating healthy food is good for you, doing so in an extreme way causes you harm. the way you’re going about it is causing harm.
The goals of psychotherapy include:
- Rethink your behavior: This means understanding the negative effects of your actions so you can change what you’re doing.
- Rewire your thoughts: Cognitive reframing helps you identify habits and beliefs that cause stress and replace them with less rigid thoughts.
- Readjust your exposure and response: The more you’re exposed to the foods or the food scenario that causes you anxiety, the less it’ll upset you over time.
- Regain your relaxation: Supplemental treatments often involve relaxation training such as breathing exercises, guided imagery, mindfulness meditation, yoga, and tai chi.
3 key things to know about orthorexia
- Good intentions can become obsessive: When you really listen to a person with orthorexia, as we do at SunCloud Health, what often drives them is their fear of cancer, heart disease, or another chronic disease that involves lifestyle risk factors such as tobacco use, poor diet, lack of exercise, or alcohol use. Our patients often admit to pouring over the internet searching for information on those factors, and how dietary changes can offer protection. People search for what causes inflammation in the body. They read articles that say to avoid sugar, avoid gluten, avoid dairy, and avoid meat. Then they take all that to the extreme.
- There’s a minefield out there called Instagram. And another one is called Twitter. And TikTok. And Facebook. Point being, big tech has algorithms that specifically target adolescents and adults who are at high risk of body dissatisfaction and eating disorders. This exploits vulnerable people who then find fault with their bodies and search for diets that will “fix” those imperfections. This greatly increases their risk of developing eating disorders like orthorexia—not to mention just making people feel terrible about themselves. Vulnerable adolescents and adults get hooked on one of these social media platforms, and search in vain for cures, answers, likes, followers, validation, and happiness.
- The thin ideal is toxic. This ideal, which has been perpetuated by our culture, product marketing, and the advertising industry for decades. Thin equals ideal and powerful. This enduring mindset systematically oppresses people of size, particularly women.
It’s also part of what makes orthorexia so difficult to deal with. It’s driven by a social construct that is baked into our healthcare system: thin equals good. This construct is all about placing thin bodies at the center of power, influence, and beauty, and rejecting all other alternatives and variations as “less than.”
Final thought: Know that long-term recovery is possible
As with many mental illnesses—depression, anxiety, and substance use disorder among them—recovery from orthorexia takes time. You don’t go to the clinic for it, get your meds and therapy, then go on your way—cured! For some people, it is a chronic condition, so you need to look after it long-term. For other people, treatment is curative.
The great news is, most people recover from orthorexia and re-establish their normal, healthy relationship to food. To help ensure this happens, I recommend ongoing therapy with a mental health professional who has specialized expertise in and experience with eating disorders. These professionals are equipped to help you re-establish normal eating habits and develop new coping skills.
Some people also benefit from going to Eating Disorders Anonymous (EDA) meetings and other support groups. For listings of these and other therapy and support resources, contact the National Eating Disorders Association (NEDA) or the National Alliance on Mental Illness (NAMI).
Get Help Now
Thinking about seeking help or know someone who does? Click below to have one of our professional team members contact you.
[one_third]Schedule a One-on-One Consultation[/one_third][one_third]Learn More About SunCloud Health[/one_third][one_third_last]Get information on Costs and Insurance[/one_third_last][/ctabar]